Home / Opioid Halo
Opioid Halo

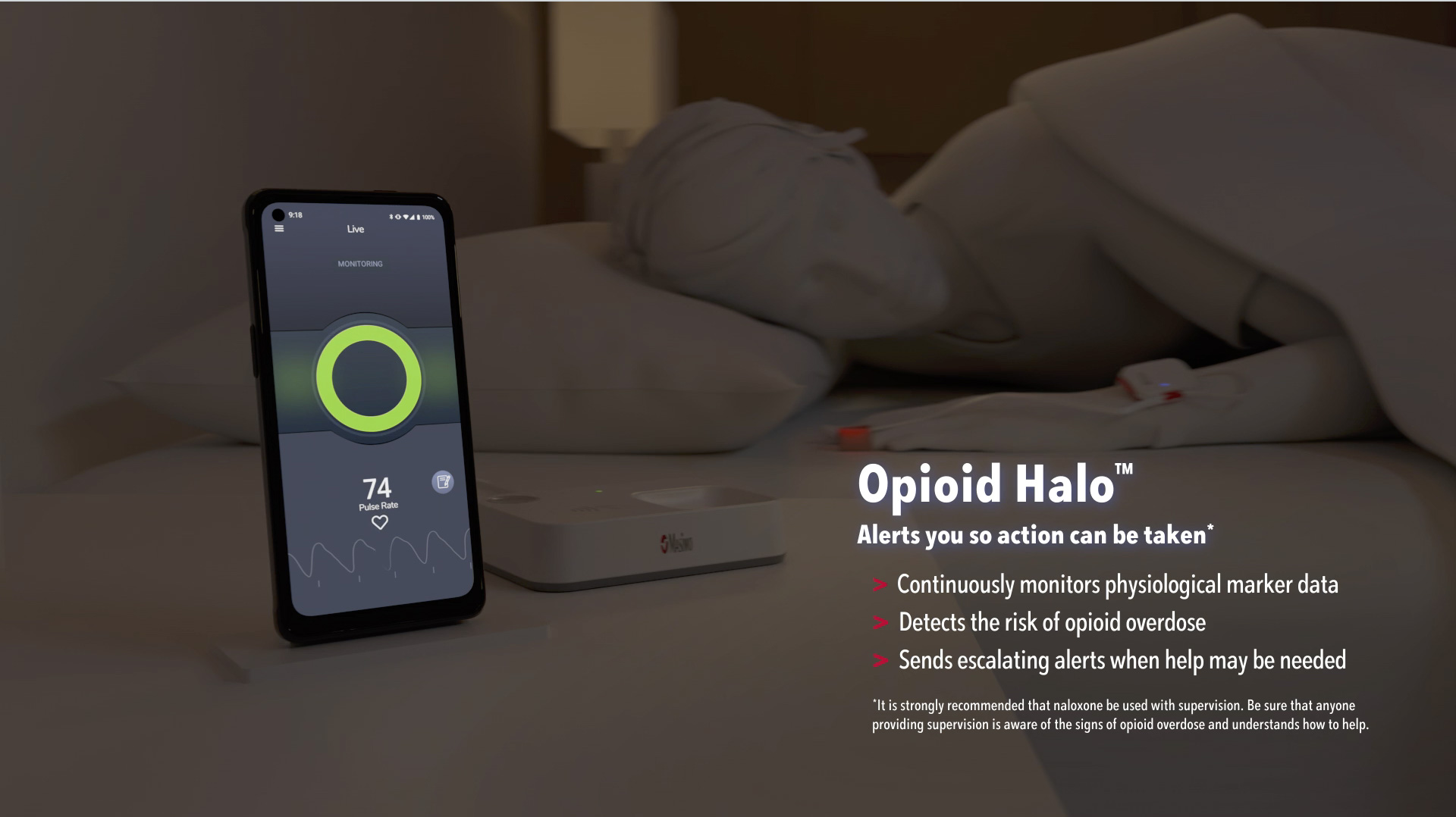
Opioid Halo™
Opioid Overdose Prevention & Alert System
Help Your Patients Create a Halo of Protection
You've educated your patients about the potential side effects of opioids, including opioid-induced respiratory depression. Now you can provide them with an extra layer of protection in case of an accidental opioid overdose emergency.
Opioid Halo provides critical monitoring for your patients to get help.*

First and only FDA-authorized device to alert you in the event of an opioid overdose

Selected for the FDA Opioid Innovation Challenge

Granted "breakthrough" device status
Opioid Halo
Opioid Overdose Prevention & Alert System

- Provides real-time monitoring to identify the risk of opioid-induced respiratory depression
- Sends escalating alerts to the patient and their designated emergency contacts, followed by an automated wellness call that may lead to EMS being dispatched
- Powered by Masimo SET® pulse oximetry, which is trusted by 9 of the top 10 U.S. hospitals1
Some patients may be at higher risk for accidental overdose
Some patients may be at higher risk for accidental overdose
Certain factors can increase risk:2-5
- Being opioid naïve
- Respiratory condition(s) such as sleep apnea
- Combining opioids with other sedating medications such as benzodiazepines and/or alcohol
- Older age (65+)
- Taking medical high prescribed doses (>50 MME)
- Medical conditions such as HIV, liver or lung diseases, or mental health conditions
- Opioid use disorder or a history of addiction
- Taking opioids for nonmedical purposes
- Taking opioids again after stopping for an extended period of time
>80,000
opioid-related deaths in 2021.6
Over 200 people are dying every day.
>20%
of opioid deaths in 2020 involved a prescription opioid.7
>50%
of opioid-related deaths occur when the person is alone.8
But even if they are not, it may be hard for a patient or their loved one to recognize the signs before it’s too late.9
Are your patients using naloxone?
Are your patients using naloxone?
Complement naloxone (e.g. Narcan®) with monitoring
Naloxone is an effective tool for overdose reversal. However, it cannot be self-administered during a low-oxygen level event.10 Continuous monitoring can be a powerful complement to naloxone by raising awareness when help is needed.
Provide a simple way to help increase patient safety
Provide a simple way to help increase patient safety
The Opioid Halo system includes:
- Intuitive mobile app

- Home Medical Hub with audible alarms

- Comfortable, disposable sensor
Help patients and their caregivers know when to take action
Help patients and their caregivers know when to take action
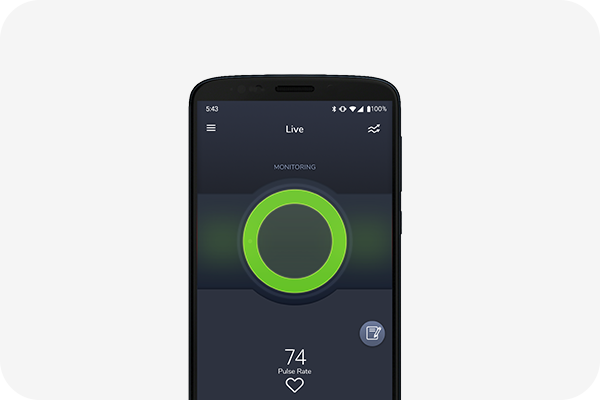
Opioid Halo uses an advanced pattern recognition algorithm to detect high or increasing risk of severe opioid-induced respiratory depression and send escalating alerts when help is needed.

Monitoring is active
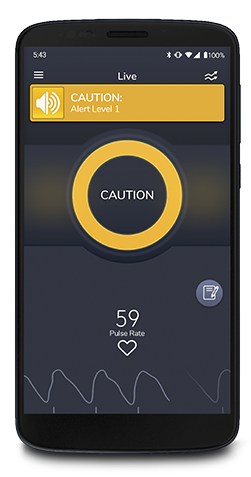
Alert 1: Caution
When physiological marker data shows high risk for overdose, alerts appear visually on the patient's mobile device and sound audibly at the Home Medical Hub, to facilitate self recovery.
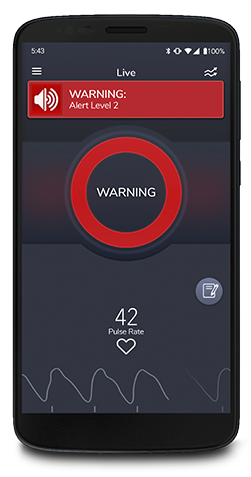
Alert 2: Warning
As the risk level rises, the system alerts them again and sends automatic texts to designated emergency contacts.†

Alert 3: Emergency
If the risk level continues to worsen, the system triggers an automated wellness call that may lead to EMS being dispatched.
Powered by clinically proven pulse oximetry
Powered by clinically proven pulse oximetry
Masimo SET® Pulse Oximetry
- Trusted by physicians for over 25 years and used to monitor over 200 million patients a year around the world11
- Features multiple parallel signal processing engines for accurate and reliable readings
- Demonstrated significantly fewer false alarms and more true alarms than conventional pulse oximetry technologies in hospital settings12
- Accurate across all skin pigmentations13
Based on a Proven Hospital Approach
A 10-year study at Dartmouth-Hitchcock Medical Center found zero opioid-related preventable deaths or brain damage in hospitalized patients who were continuously monitored with Masimo SET® and a notification system.14
Opioid Halo leverages the same clinically proven pulse oximetry technology and a similar notification system to help protect your patients at home.

Try Opioid Halo Today
Contact us for an in-office demonstration and see how Opioid Halo can help protect your patients while taking opioids.
RESOURCES
References
- 1.
Masimo SET® is the primary pulse oximetry at 9 of 10 top U.S. hospitals as ranked in the 2022-23 U.S. News and World Report Best Hospitals Honor Roll, available at:
https://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview. - 2.
CDC.
https://www.cdc.gov/opioids/providers/prescribing/pdf/identifying-opioid-risk-factors.pdf. - 3.
Opioid Overdose.” World Health Organization, 28 Aug. 2020,
www.who.int/news-room/fact-sheets/detail/opioid-overdose. - 4.
Gupta K et al. Curr Opin Anaesthesiol. 2018;31(1):110-119.
- 5.
Dunn KM et al. Annals of internal medicine. 2019;152(2):85-92.
- 6.
National Center for Health Statistics. CDC.
https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm. - 7.
National Center for Health Statistics. CDC.
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6101a3.htm. - 8.
Public Health Ontario. Opioid Mortality Surveillance Report.
https://www.publichealthontario.ca/-/media/documents/opioid-mortality-surveillance-report.pdf?la=en. - 9.
Opioid Overdose.” World Health Organization, 28 Aug. 2020,
www.who.int/news-room/fact-sheets/detail/opioid-overdose. - 10.
Lifesaving Naloxone. CDC.
https://www.cdc.gov/stopoverdose/naloxone/index.html. - 11.
Estimate. Masimo data on file.
- 12.
Shah et al. J Clin Anesth. 2012;24(5):385-91.
- 13.
Barker S.J. et al. J Clin Monit Comput (2022). Available online at:
https://doi.org/10.1007/s10877-022-00927-w. - 14.
McGrath S et al. J Patient Saf. 2020 14 Mar. DOI: 10.1097/PTS.0000000000000696.
-
* It is strongly recommended that naloxone be used with supervision. Be sure that anyone providing supervision is aware of the signs of opioid overdose and understands how to help.
† Emergency contacts must agree to receive alerts.
iOS is a trademark or registered trademark of Cisco in the U.S. and other countries and is used under license. ANDROID™ is a registered trademark of Google Inc. Bluetooth word mark and logos are registered trademarks owned by Bluetooth SIG Inc.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. See instructions for use for full prescribing information, including indications, contraindications, warnings, and precautions.
The Bluetooth® word mark and logos are registered trademarks owned by Bluetooth® SIG, Inc. and any use of such marks by Masimo is under license.
PLCO-006624/PLM-13845A-0323